The role of the private sector with respect to health issues has long been contested in academic and policy debates. Should employers be trusted to act as socially responsible citizens and take steps to support improvements in health for their workers and wider society, or does the state have to step in to enforce good practices through regulation?
This ongoing debate has significant implications in the context of the HIV epidemic in sub-Saharan Africa, given the mistrust of the state by foreign donors, and years of under-spending on healthcare systems following structural adjustment policies imposed across the continent in from the mid 1980s onwards, and more broadly during the era of Neoliberalism.
The business case for intervention
In this setting, it is hoped that employers can be encouraged to support the struggle against HIV by persuading them that there is a good business case for doing so. The business case for intervention rests on a Cost-Benefit Analysis approach which weighs up the potential costs avoided by firms that have HIV positive employees in their workforce (such as workers being off sick, reduced productivity, higher staff turnover, higher recruitment and training costs, and increased healthcare benefit payments) against the costs of implementing a workplace HIV programme (which can include the provision of Voluntary Counselling and Testing services, access to Antiretrovirals, education and communication campaigns and peer-to-peer support).
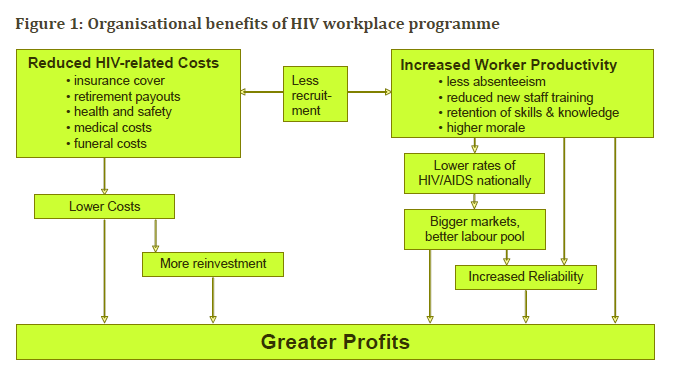
Image credit: https://www.popline.org/node/198172
In some cases, evidence suggests that the potential savings (i.e the benefits) far outweigh the costs of the workplace programme, and it is assumed that employers will therefore respond to this evidence in a 'rational' way by implementing workplace programmes.
However, on closer inspection, the evidence is narrow and incomplete, with the business case holding for a limited number of formal sector skilled workers, but not for workers in informal and casual employment, who are a majority across sub-Saharan Africa. The evidence is also dominated by case studies that focus on sectors such as mining, a sector highly implicated in the spread of HIV, and blue chip companies which again do not represent the employment experience of the majority of the population in sub-Saharan Africa.
Alternative strategies to address HIV related costs
Further, the Cost-Benefit Analysis approach fails to incorporate alternative strategies that Firms may employ to address HIV related costs, such as pre-employment screening, managing HIV positive workers out of the business, cutting healthcare benefits, and a trend towards more casualised labour contracts in which the costs of the epidemic are shifted onto workers, their families, and the state.
The result, unsurprisingly, is a limited response by firms to the issue of HIV. Relying on persuading employers that investing in HIV programmes for their workers makes good business sense has not stimulated the desired response. This suggests that policy makers need to create conducive conditions for positive responses through enhanced regulation, in addition to - not in replacement of - strengthening public healthcare systems.
Ready to discover how the Queen Mary Online MSc in Global Public Health can help you achieve your career goals?
About the author
Dr Kevin Deane is a Lecturer in Global Public Health at Queen Mary, and Co-Coordinator of the Queen Mary Online MSc Global Public Health.
For a more comprehensive discussion of this topic see:
Deane K, Stevano S, Johnston D (2019), Employers' responses to the HIV epidemic in sub-Saharan Africa: Revisiting the evidence. Development Policy Review, Vol 37, pages 245-259. https://doi.org/10.1111/dpr.12380
.png?width=280&height=74&name=logo%20(1).png)


 Follow us on Twitter
Follow us on Twitter Like us on Facebook
Like us on Facebook